‘Special’ cattle antibodies may lead to HIV vaccines and therapeutics
“Cows do neat things,” said Michael Criscitiello, an associate professor in the Texas A&M College of Veterinary Medicine & Biomedical Sciences’ Department of Veterinary Pathobiology as he sat in his office one Friday afternoon.
For the past six years, Criscitiello has been taking advantage of, arguably, one of the neatest things that cows can do.
Using “special antibodies” that cows naturally produce, Criscitiello and a team of researchers (including at Scripps Research Institute) have made significant headway in HIV research by eliciting broadly neutralizing antibodies to the virus that biomedical engineers in California and New York believe may hold a key for HIV vaccines, therapeutics, or other prevention tools.
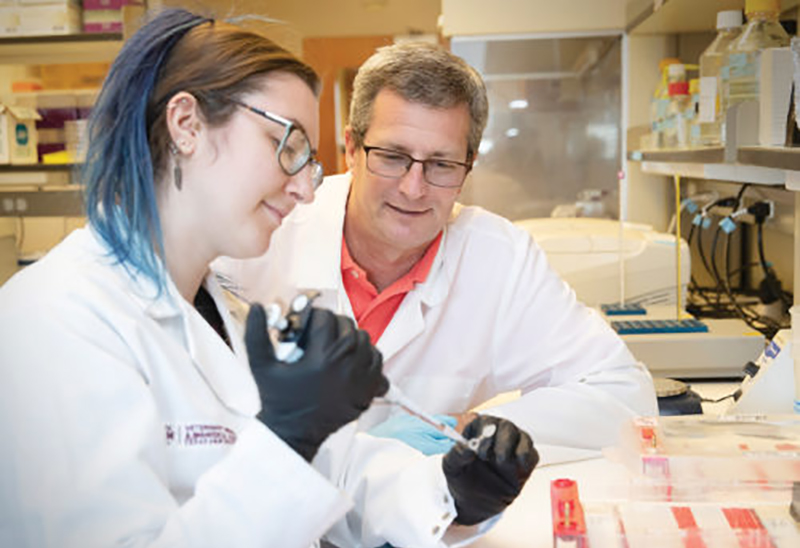
While that project has advanced into the human medicine realm, Criscitiello and another team, including master’s student Kelly Head, are now turning their attention to using these same antibodies in a way they hope might one day be used to create an immunological treatment for breast cancer.
Both projects began by immunizing a cow.
A comparative immunologist who has devoted his career to studying “weird” antibodies in vertebrates—including sharks and frogs—Criscitiello observed a remarkable phenomenon that appears in cattle antibodies.
“About 15 percent of cow antibodies have this extra finger-like projection; we call it an extra domain of the protein that’s not in our antibodies,” he said. These projections are called heavy chain complementarity-determining region 3, or HCDR3 loops.
While humans don’t have the immunogenetic tools to make HCDR3 in our genome, HIV researchers found that 10 to 20 percent of people living with HIV do, indeed, naturally develop neutralizing antibody responses similar to HCDR3, but usually only after nearly two years of infection.
The human forms of the projections have been shown in the laboratory to stop most HIV strains from infecting human cells and to protect animal models from infection, which occurs when the antibody projection binds to the gp120 antigen of the virus that it uses to attach to the host white blood cell.
Using this research as a frame of reference, and noticing how cow antibodies have this much, much longer extension, Criscitiello and his team postulated that this HCDR3 loop could possibly bind to the virus more effectively.
“In a nutshell, the cow can make an antibody that can reach a part of the virus that our antibodies normally can’t,” Criscitiello said.
In order to test the theory that these broadly neutralizing antibodies (which include the HCDR3 loop) could potentially serve as a pathway to produce an immunological therapy, or possibly even a vaccine, for HIV, researchers would need more of these broadly neutralizing antibodies and they would need them to be produced rapidly, at a scale suitable for widespread distribution.
So, Criscitiello and a team at Texas A&M went to work, immunizing cows with a protein designed to mimic an HIV surface protein to see if the cow would produce an immunological response, creating antibodies with these HCDR3 loops.
“What was exciting was that we found that the cows didn’t just make a good antibody; they made lots of antibodies, and those antibodies bound not just some HIV very well but they were broadly neutralizing all different forms of the virus from all over the world,” Criscitiello said.
In addition, the cattle produced those antibodies a lot faster than the team had anticipated.
“Usually, it takes six to eight months (to see an immunological response), because we give them boosters, the way you do with some vaccines,” Criscitiello said. “But we actually had really good antibodies in a couple months.”
Since the team published their results, medical engineering companies have picked up the research, using DNA cloning that attempts to take the part of the cattle gene that produces the HCDR3 loops and put that piece of DNA into a human antibody-heavy chain.
The result, he says, would likely be a therapy to serve as “first line of defense,” but the therapy would be an immunological therapy instead of a medical treatment. A lot of testing will go into the clinical intervention stage, but Criscitiello says the research is promising.
“This is exciting for our lab, as our work is generally on more fundamental immunology questions and takes longer to be applied into therapeutic interventions,” Criscitiello said.

